
By Warren R. Heymann, MD
March 18, 2020
Vol. 2, No. 11

Disclaimers: This commentary was written on March 12, 2020 for a publication date of March 18, 2020. The issues related to the COVID-19 pandemic are changing at breakneck speed. The content included in this commentary may no longer be factual or relevant by the publication date. The reader is encouraged to stay abreast of developments via the CDC and local government and institutional health care authorities.
March 18, 2020 has been circled on my calendar for months, as I was eagerly anticipating my trip to Denver for the Annual Meeting of the American Academy of Dermatology. I have been to every meeting since finishing my residency in 1983 and was excited to lecture, learn, work on committees, mingle with old and new friends, and dine with gusto. I had actually made the excruciating decision to forego the meeting prior to the official cancellation, not so much for fear of contracting COVID-19, but to avoid the risk of a quarantine. I applaud the President of the AAD, George Hruza, and the AAD Board of Directors for making the painful, but correct, decision to cancel the Denver convention for the safety of all.
I can only imagine what the world experienced with the 1918 influenza pandemic. Now we are experiencing a global health crisis in real time with real consequences. Bill Gates offers an appropriate perspective: “We need to save lives now while also improving the way we respond to outbreaks in general. The first point is more pressing, but the second has crucial long-term consequences.” (1) This commentary focuses on immediate concerns.
COVID-19 was recognized in December 2019. It was rapidly shown to be caused by a novel coronavirus that is structurally related to the virus that causes severe acute respiratory syndrome (SARS). (2) In their review of 1099 cases of COVID-19 infection from mainland China, Guan et al reported that during the first 2 months of the outbreak, COVID-19 spread rapidly throughout China causing varying degrees of illness. Importantly, patients often presented without fever, and many did not have abnormal radiologic findings. “The median age of the patients was 47 years; 41.9% of the patients were female. The primary composite end point occurred in 67 patients (6.1%), including 5.0% who were admitted to the ICU, 2.3% who underwent invasive mechanical ventilation, and 1.4% who died. Only 1.9% of the patients had a history of direct contact with wildlife. Among nonresidents of Wuhan, 72.3% had contact with residents of Wuhan, including 31.3% who had visited the city. The most common symptoms were fever (43.8% on admission and 88.7% during hospitalization) and cough (67.8%). Diarrhea was uncommon (3.8%). The median incubation period was 4 days (interquartile range, 2 to 7). On admission, ground-glass opacity was the most common radiologic finding on chest computed tomography (CT) (56.4%). No radiographic or CT abnormality was found in 157 of 877 patients (17.9%) with nonsevere disease and in 5 of 173 patients (2.9%) with severe disease. Lymphocytopenia was present in 83.2% of the patients on admission.” Only 2 patients (0.2%) had a “rash.” (3)
Cutaneous manifestations of COVID-19 may be rare but no other disease has ever had a more profound effect on dermatologists and their practices.
The goal of every institution (medical or otherwise), practice, physician, patient, and human being is to do whatever is necessary to slow the spread of the virus. The purpose of this is twofold — to avoid infecting another person individually and also try to keep illness at bay so that the health care system is not overwhelmed. The outbreak in Italy is a prime example of hospitals in crisis mode, unable to handle the burden of disease. The lack of ventilators has provided Italian physicians an unenviable moral dilemma of choosing who shall live or die. Mounk observes “… the Italian College of Anesthesia, Analgesia, Resuscitation and Intensive Care (SIAARTI) has published guidelines for the criteria that doctors and nurses should follow in these extraordinary circumstances. The document begins by likening the moral choices facing Italian doctors to the forms of wartime triage that are required in the field of ‘catastrophe medicine.’ Instead of providing intensive care to all patients who need it, its authors suggest, it may become necessary to follow ‘the most widely shared criteria regarding distributive justice and the appropriate allocation of limited health resources.'” (4) The heartbreaking tragedy is that if there were adequate ventilators available such choices would not be necessary. I am saddened to predict that many Italian physicians who have made these decisions will be dealing with post-traumatic stress disorder in the pandemic’s wake.
Varun Verma, the hospitalist medical director at Jefferson Cherry Hill Hospital in New Jersey, where our initial local COVID-19 patient was admitted, offers the following advice to patients, aside from “don’t panic.” “Of course, we should all stay at home if sick, wash our hands carefully, not divert face masks from frontline health-care workers, and we should pay special attention to the elderly and vulnerable. Additionally it serves as an excellent reminder to review our emergency preparedness plan on ready.gov.” (5) I looked at the website and it offers simple, outstanding recommendations for pandemic preparation. Rescheduling appointments for elderly patients older than 65, especially those with underlying morbidities such as diabetes or congestive heart failure, should be a priority. (Two personal questions arise: 1) I turn 65 in May — does that make me elderly? 2) If we are asking patients of that age to stay home, should I be asking myself to not see patients?)
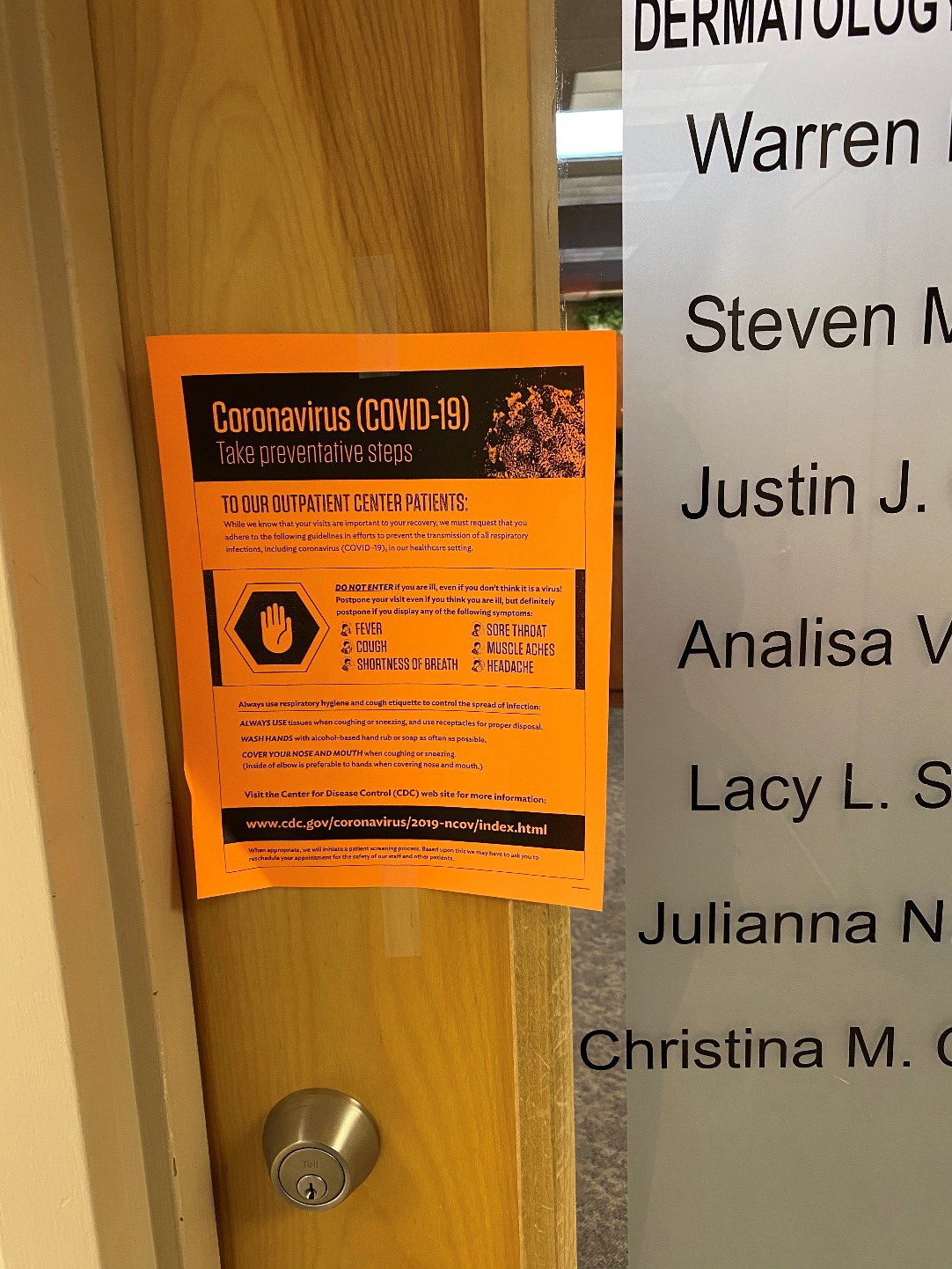
Our practice has changed dramatically this past week. There have been many canceled appointments. We have placed a sign on our door warning patients of COVID-19 and asking them not to enter if they are displaying flu-like symptoms (see image). We are changing our recorded confirmation message to reflect this request. I have changed my habit of shaking every patient’s hand — which I would often do in a Bill Clintonesque two-handed manner — to a friendly greeting. On a lighter note (and we really need that!), it took me a couple of days to get comfortable with how I would greet patients without a handshake. An air handshake honestly felt ridiculous, fist bumping makes no sense if you are trying to avoid contact, bumping elbows may not be the best approach if we are asking patients to cough or sneeze on their arm if they must, and bowing Japanese style felt awkward. I decided to bow as I was taught in kindergarten, right arm to the front, and left arm to the back. Patients loved it. Some even responded with a curtsy! Additionally, although anxious, patients seem a little friendlier, and possibly even more concerned about the world at large. For those who ask me when I’m thinking about retiring, I tell them with the stock market tanking on a daily basis – “when I die.” They smile.
Cancellations are wreaking havoc for the NBA, NCAA, MLB, universities, public schools, houses of worship, conferences, and anywhere where communities gather. For any working parents of school-age children, dermatologists included, this may present a logistical nightmare.
There have been recent publications highlighting how dermatology departments have been organizing themselves in the midst of COVID-19. Triage, hand hygiene, N-95 masks, and coordination following local infection control policies is essential. (6) On Jan. 24, 2020, West China Hospital of Sichuan University temporarily closed the doors of the dermatology outpatient department and dermatology surgery by postponing all the elective surgeries and only limiting to emergency operations. The department did not completely halt the services to some patients that required care during the 2019-nCoV outbreak. These patients were evaluated following appropriate triage and a two week quarantine. The doctors were required to wear masks, surgical caps, protective suits, gloves, and goggles at work, and take off their protective equipment only after their work to a designated disposable area. (7)
Dermatologists, of course, represent just one specialty facing these universal COVID-19 issues. The following is from the abstract from Lai et al with their experience as ophthalmologists. “A three-level hierarchy of control measures was adopted. First, for administrative control, in order to lower patient attendance, text messages with an enquiry phone number were sent to patients to reschedule appointments or arrange drug refill. In order to minimize cross-infection of COVID-19, a triage system was set up to identify patients with fever, respiratory symptoms, acute conjunctivitis, or recent travel to outbreak areas and to encourage these individuals to postpone their appointments for at least 14 days. Micro-aerosol generating procedures, such as non-contact tonometry and operations under general anaesthesia were avoided. Nasal endoscopy was avoided as it may provoke sneezing and cause generation of droplets. All elective clinical services were suspended. Infection control training was provided to all clinical staff. Second, for environmental control, to reduce droplet transmission of COVID-19, installation of protective shields on slit lamps, frequent disinfection of equipment, and provision of eye protection to staff were implemented. All staff were advised to measure their own body temperatures before work and promptly report any symptoms of upper respiratory tract infection, vomiting or diarrhoea. Third, universal masking, hand hygiene, and appropriate use of personal protective equipment (PPE) were promoted.”(8) With little modification, this approach is applicable to dermatologists and other specialties.
One of the potential solutions of this crisis is utilizing teledermatology to its fullest capabilities. We use an app with our EMR. To date, in our practice, I have used it the least among my partners, as I have found it disruptive to my day. Should there now be large gaps in my schedule, I may sing a different tune. Additionally, to protect hospitalist dermatologists performing inpatient consultations, teledermatology may be uniquely suitable. To date, inpatient teledermatology has been underutilized although it has the potential to increase access to dermatologic care and may be best used for triaging and remote staffing. (9) As Hollander and Carr opine: “Though telehealth will not solve them all, it’s well suited for scenarios in which infrastructure remains intact and clinicians are available to see patients. Payment and regulatory structures, state licensing, credentialing across hospitals, and program implementation all take time to work through, but health systems that have already invested in telemedicine are well positioned to ensure that patients with COVID-19 receive the care they need. In this instance, it may be a virtually perfect solution.” (10)
Most authorities predict the crisis to worsen in the coming weeks. Simply, our lives will not be the same for the near future, and perhaps, will never be the same again. When this crisis passes, hopefully many lessons will have been learned to mollify future pandemics. At times like these, where there are so many questions that must be addressed, it helps to seek the wisdom of sages past. There is no better time to heed the advice of Hillel: “If I am not for myself, who will be for me? If I am not for others, what am I? And if not now, when?”
Point to Remember: The COVID-19 pandemic is changing our lives in profound ways. Dermatologists have a responsibility to care for themselves, their families, patients, and community. With preparation and implementation of infection control measures, it is hoped that the pandemic will resolve, and that lessons learned will guide us for potential future infectious threats.
Our Expert’s Viewpoint
Misha Rosenbach, MD
Associate Professor of Dermatology
Hospital of the University of Pennsylvania
COVID-19 has the potential to be the acute, defining medical catastrophe of our time.
As always, Warren is eloquent even when covering a complex topic. Those of you who know him are probably soothed by the sound of his voice in your head reading those words. “Don’t panic” is important to remember. However, the novel coronavirus SARS-CoV-2 (COVID-19) is going to test our country, our colleagues, and our field. Infectious disease epidemiology experts have implored leaders, and the public, to “flatten the curve.” (11) This means practicing social distancing measures to delay the rate-of-rise of this exponentially expanding infection, with the goal being to avoid an overwhelming influx of patients into our hospitals that are already overtaxed by a protracted flu season. A viral social media post by Dr. Daniele Macchini from the Humanitas Gavazzeni hospital in Bergamo, Italy, painted a stark picture of the conditions there. (12) The rate of infections in the United States has closely mirrored that in Italy, though we lag 10 days behind. It is essential that we all take whatever measures are in our power to limit the rapid spread of COVID-19 and delay the impending tsunami of hospitalizations. For dermatologists, that may mean implementing measures such as:
- Canceling non-urgent outpatient visits (acne, annual skin checks, cosmetic procedures, post-operative wound checks, stable patients with chronic skin conditions, etc.)
- Implementing new phone reminders (advising patients who are febrile, with URI symptoms or a cough, or known exposure to COVID-19 to stay home)
- Implementing tele-triage or tele-medicine (Congress passed the Coronavirus preparedness and response supplemental appropriations act last week, allowing physicians and other health professionals to bill Medicare for patient care delivered by telehealth during the coronavirus emergency). (13)
- Adjusting signage in your waiting rooms (Warren’s example is a nice one), and even considering adjusting your waiting rooms (to have empty space or blank chairs to encourage distancing)
For dermatologists who practice inpatient hospital care, the Society of Dermatology Hospitalists has put out a statement recommending adjustments to standard practice, including guidelines for triaging non-urgent consults, avoiding extra visits into patients on isolation, and using telemedicine whenever possible given its studied accuracy as an inpatient triage tool. (14, 15)
Should you as a dermatologist find yourself caring for patients with COVID-19, please refamiliarize yourselves with appropriate donning and doffing of personal protective equipment. Note that due to the mechanism by which COVID-19 can be spread, eyewear is recommended, in addition to standard airborne/droplet/contact isolation precautions. The UCSF infection control department has an updated video.
Everyone, please do what you can to flatten the curve, and prevent our health care system and hospitals from being overwhelmed. Be safe, wash your hands, and take care of your patients, friends, families, and yourselves during this difficult period.
- Gates B. Responding to Covid-19 – A once-in-a-century pandemic? N Engl J Med 2020 Feb 28 doi: 10.1056/NEJMp2003762 [Epub ahead of print].
- Fauci AS, Lane HC, Redfield RR. Covid-19 – Navigating the uncharted. N Engl J Med 2020 Feb 28 2020 Feb 28. doi: 10.1056/NEJMe2002387. [Epub ahead of print].
- Guan WJ, Ni ZY, Hu Y, Liang WH, et al. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med 2020 Feb 28 doi: 10.1056/NEJMoa2002032 [Epub ahead of print].
- Mounk Y. The extraordinary decisions facing Italian doctors. The Atlantic. March 11, 2020.
- Verma V. Leaders must have courage to make tough decisions. Philadelphia Inquirer. March 12, 2020.
- Tao J, Song Z, Yang L, Huang C, et al. Emergency management for preventing and controlling nosocomial infection of 2019 novel coronavirus: Implications for the dermatology department. Br J Dermatol 2020 Mar 5. doi: 10.1111/bjd.19011. [Epub ahead of print].
- Chen Y, Pradhan S, Xue S. What are we doing in the dermatology outpatient department amidst the raging of 2019-nCoV? J Am Acad Dermatol 2020 doi: 10.1016/j.jaad.2020.02.030. [Epub ahead of print].
- Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol 2020 Mar 3 doi: 10.1007/s00417-020-04641-8. [Epub ahead of print].
- Weig EA, Tull R, Chung J, Wanat KA. Inpatient teledermatology: Current state and practice gaps. J Am Acad Dermatol 2019 Jul 12 doi: 10.1016/j.jaad.2019.07.013. [Epub ahead of print]
- Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020 Mar 11. doi: 10.1056/NEJMp2003539. [Epub ahead of print].
- Siobhan Roberts, Flattening the Coronavirus Curve. The New York Times, March 11, 2020 – accessed online 3/12/2020.
- Daniele Macchini, We are all just doctors trying to fight this tsunami that crashed on us. As reported in The Telegraph, March 10, 2020 – accessed online 3/12/2020
- Kent Moore, AAFP.org, March 10, 2020 – accessed online 3/12/2020 https://www.aafp.org/journals/fpm/blogs/gettingpaid/entry/coronavirus_testing_telehealth.html
- Barbieri JS, Nelson CA, James WD, et al. The reliability of teledermatology to triage inpatient dermatology consultations. JAMA Dermatol 2014;150(4):419-24.
- Rosenbach M @MishaRosenbach. “@Dermhospitalist guidelines for inpatient dermatology during Covid-19.” 3/12/2020 12:26pm EST. Tweet.
All content found on Dermatology World Insights and Inquiries, including: text, images, video, audio, or other formats, were created for informational purposes only. The content represents the opinions of the authors and should not be interpreted as the official AAD position on any topic addressed. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
